This blog was written in collaboration with Dan Newingham, Solution Delivery Manager, ZS and Aaron Zavora, Technical Director, HLS, Databricks
Mandates for electronic prior authorization along with evolving reimbursement patterns due to Value Based Care (VBC) arrangements are changing how health plans approve services for members. There exists a tremendous opportunity to leverage data across a growing number of use cases that will deliver on improved patient outcomes, help fend off a growing administrative problem around prior authorization, and deliver a meaningful ROI for the business.
The growing prior authorization problem
Prior Authorization is a program implemented by health plans to ensure proper utilization of healthcare services such as procedures, prescriptions, and durable medical equipment (DME). These programs are designed to reduce unnecessary services while still maintaining quality outcomes for patients. The balance of restricting services while ensuring quality patient outcomes can be difficult to measure without the use of data & AI.
Compounding this challenge is that across the healthcare ecosystem payers and providers are seeing prior authorization as a growing operational problem. In 2022 alone, transaction volume increased by 61% and the cumbersome manual review process consumes hundreds of millions of dollars each year. Despite a frenzy of regulatory initiatives, the problem is not expected to subside on its own, at least not while membership continues to grow in plans that require prior authorizations such as Medicare Advantage, which are experiencing double digit annual growth.
The potential ROI of advanced analytics and AI/ML in PA operations
To get ahead of the growing prior authorization problem, health plans must implement creative ways to optimize prior authorization operations. Fortunately, there are several proven use cases for advanced analytics and AI/ML across intake, review, and approval that can help alleviate the pain as well as bring a compelling ROI for the business.
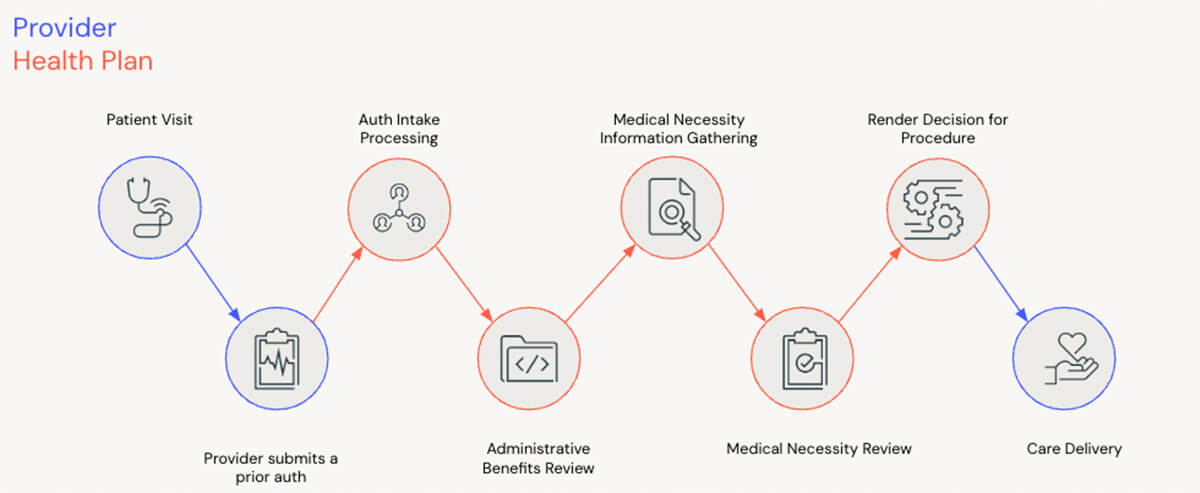
Optical Character Recognition (OCR) for Intake: Despite progress towards electronic prior authorizations, most authorizations continue to be submitted manually via fax or email. Unfortunately, we cannot expect all providers to transition to a fully electronic workflow overnight so health plans can still benefit by using OCR for converting manual submissions to electronic submissions. An appropriately tuned model can reduce manual intake effort up to 72%1.
Large Language Models (LLMs) for Administrative Review: LLMs excel at sifting through the vast volumes of messy, unstructured data that typically represent member benefits. Today, health plans rely on a process of manual benefit review that can be greatly reduced with the workforce augmentation capabilities of LLMs. With the right approach to prompt engineering, an LLM can increase administrative benefit review tasks.
Predictive Models for Auto-Approval: The medical necessity review is often the most expensive step of the prior authorization process. Fortunately, it is also a great use case for the application of predictive models. With years of historical determinations data available in-house, a predictive model to assist with medical necessity review can be quickly and accurately trained. An appropriately tuned model can reduce medical necessity review effort up to 80%2.
Value Based Care Alignment: Health plans implement programs designed to reward providers for consistent, quality outcomes for patients and even engage in financial joint ventures for cost of care (e.g. narrow networks). Unifying data across VBC and utilization programs prioritizes medical necessity reviews and can reduce effort needed for your network of high performing physicians.
How health plans can prepare for AI driven prior authorization
To succeed in modernizing prior authorization operations through analytics, health plans must coordinate efforts across business and IT stakeholders. This requires communicating a broader prior authorization vision that effectively illustrates how emerging technology capabilities can transform existing PA workflows and drive real ROI. Tactically, health plans can start their journey to AI driven prior authorization through the following actions:
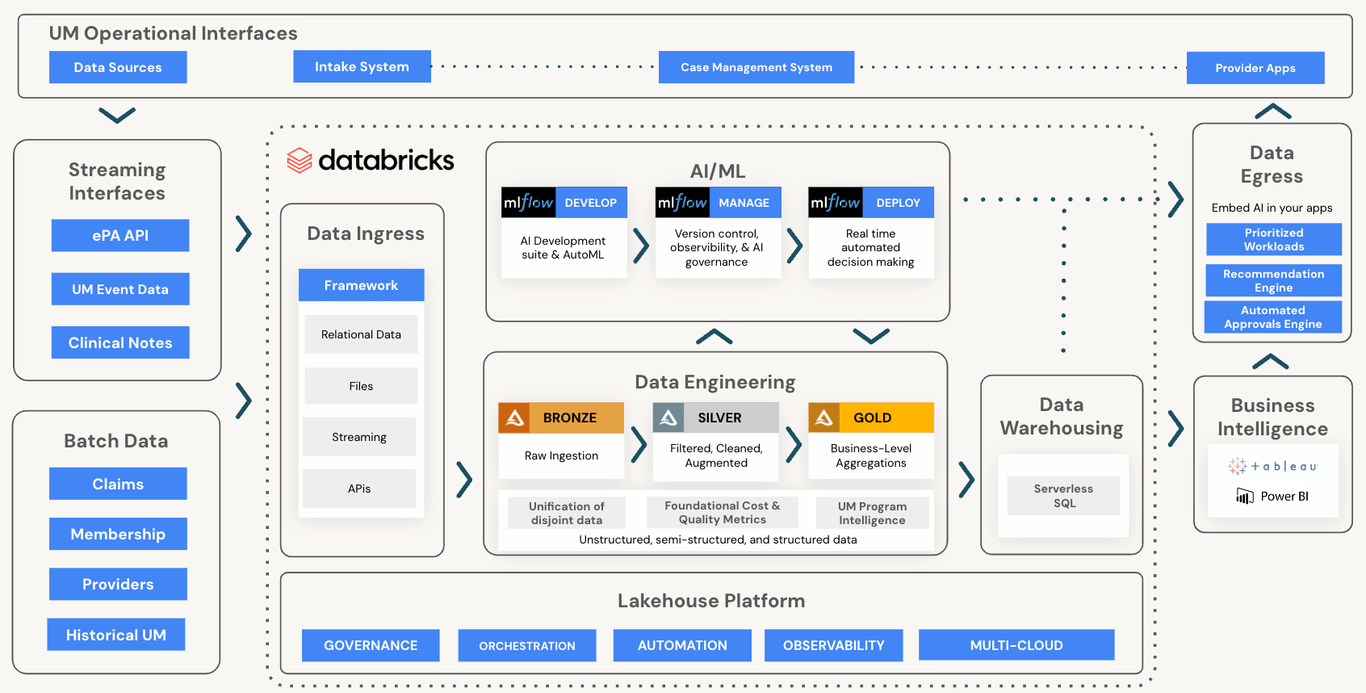
- Select a technology that will lay the right foundation of analytics infrastructure, supporting structured and unstructured data, batch and streaming, unlimited scale, and best in class AI that can be operationalized to drive automated decision making.
- Identify a vendor or partner who understands the domain and provides accelerators that will reduce the time to market for AI use cases.
- Invest in building data products, including Prior Authorization data that increases visibility and transparency into your current state of operations and pain points.
- Build a proof of concept to pick the analytics use case(s) that are right for your stakeholders and business.
- Deploy validated concepts at scale with governed data and AI capabilities and automated monitoring.
Databricks and ZS have partnered together to bundle the technology platform capabilities and domain expertise required for health plans to hit the ground running. Analytics use cases to monitor utilization management program performance and operational workflows can easily be implemented on a single platform alongside efficiency driving AI/ML models.
Setting the stage for what’s next
The Centers for Medicare & Medicaid Services (CMS) has taken a first step toward automating PAs by introducing a mandate to exchange PA transactions using APIs. In reality, a simple lift and shift of the existing manual processes will not lead to any meaningful improvements, and with the growing operational burden of prior authorization, health plans cannot afford to settle for the status quo.
While bringing advanced analytics and AI into prior authorization operations can feel overwhelming, plans will benefit from establishing the appropriate infrastructure today. Every step should provide incremental value and help plans remain agile in an evolving business and regulatory environment.
Databricks & ZS have partnered together to help customers address the aforementioned challenges and transform the Prior Authorization workflow with data & analytics.
To learn more about how to get started, connect with us.
1 https://www.caqh.org/sites/default/files/2022-caqh-index-report%20FINAL%20SPREAD%20VERSION.pdf
2 https://www.caqh.org/sites/default/files/2022-caqh-index-report%20FINAL%20SPREAD%20VERSION.pdf